I’m pretty sure you have heard about how important is gut health.
Our microbiota consists of a vast array of microorganisms, including bacteria, protozoans, yeast, and archaeans. These microorganisms are present throughout our body, with distinct microbiota residing on our skin, in our lungs, in our genital area, and most notably, in our gut (which we will focus on studying).
When our microbiota thrives and lives contentedly within us, we enjoy a harmonious symbiotic relationship. We support it, and in turn, it supports us. Neglecting its well-being can lead to it becoming adversarial. Today, we shall explore various ways in which our gut microbiota engages with us.
Where does gut health intervene in our body?
The microbiota is present in our whole lives from the moment of conception. It can even be one problem to become pregnant, some antibiotics and resolved if it’s the case. Have you heard about gestational diabetes? Well, the gut microbiota manipulates the mother’s metabolism to favor itself.
Now let’s see how it can affect us in our normal lives.
Even if you’re not aware of its name, chances are you’ve used classical conditioning before. It involves teaching someone or an animal to associate a certain event or stimulus with a specific outcome. For instance, let’s say you take your son to the park every evening (the initial stimulus) and buy him an ice cream (the outcome).
Over time, your son links going to the park with getting ice cream. He becomes increasingly expectant of the treat. However, if one day you decide not to buy the ice cream, or cannot do so, your son will feel disappointed. Depending on his age and level of understanding, he might even throw a tantrum.
What is the connection between parks and ice-cream that we are discussing? There is a unique relationship between our gut microbiota and ourselves, where one can influence the other.
In those who suffer from Inflammable Bowel Disease, some species of Lactobacillus when exposed to sugar manipulate opioid and cannabinoid receptors. They can give a “morphine boost” to their host. A little boost here, another there, and addicted to sugar!
Another example connected to sugar is germ-free mice. These mice are born by cesarean and kept in a sterile environment, that means that they don’t have microbiota. These germ-free mice have super taste buds attuned to sugar. They become addicted much easier than normal mice (with healthy gut microbiota). We can say that sugar cravings are a symptom of an unhealthy gut (dysbiosis). (1)

On the flip side, we have a symbiotic relationship with a beneficial bacteria called Bifidobacterium. When we consume insoluble fiber and it reaches our colon, these Bifidobacterium can break it down (assuming we are in good health). As a result, Bifidobacterium produce butyrate, a substance that nourishes and heals our gut, enhances our mood, reduces inflammation, and may even boost the growth hormone in our brain. Truly captivating.
That’s why we recommend avoiding sugar and increasing fiber in or diet. You can learn more about the best steps for an optimal gut health here.
As we can observe, there is a direct correlation between our gut health and our nervous system. The connection is so strong that the number of neurons near the digestive system matches those in the Central Nervous System. These neurons encompass our digestive system, acquiring knowledge and sensations. This intricate network of gut neurons transforms our gut microbiome into what can be deemed as our “Second Brain”. We will see more about the gut-brain axis another time.
Not all relationships with gut microbiota are good or bad.
We have Helicobacter pylori, Escherichia coli, among others. We know H. pylori as bacteria that causes ulcers, especially if we are stressed. H. pylori is spiral shaped, it takes advantage of it to borrow into the gastric mucus, making the stomach its home. It weakens the stomach’s protective mucus layer and proceeds to multiply, leading to a painful infection. Elders that have had a pylori infection are more prone to develop gastric cancer.
On the other hand, it is interesting to discover that having a healthy amount of H. pylori in our system can actually protect against asthma. Furthermore, ongoing research suggests that it may also have a protective effect against gastric cancer.
Most of us have H. pylori living in our stomachs right now. Why aren’t we ill?
Well, it depends on the status of our stomach.
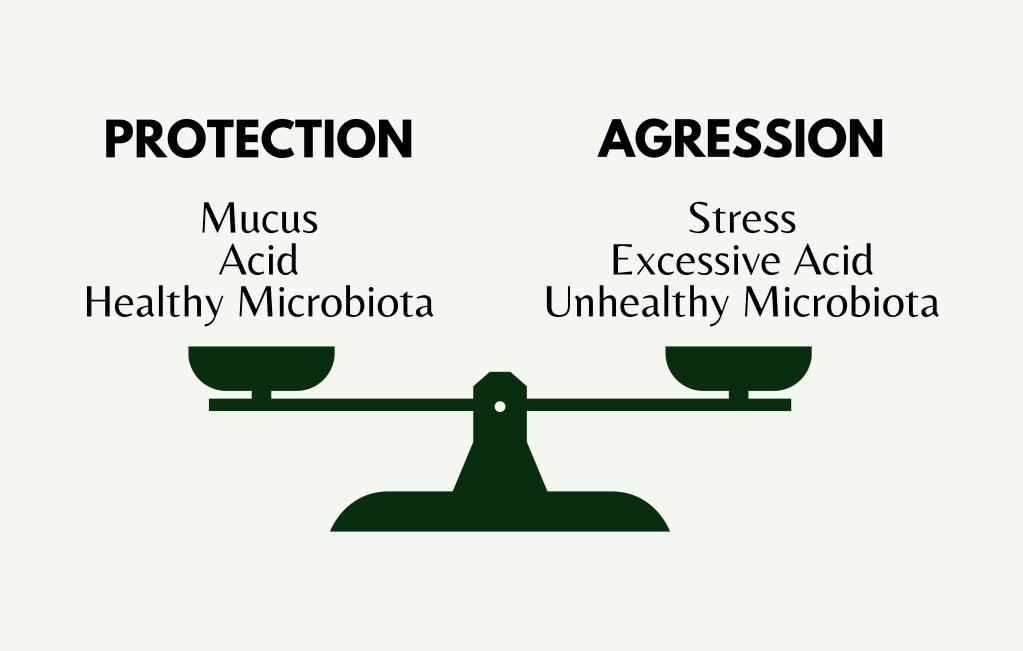
Typically, our stomach is shielded against external pathogens by its mucus, healthy microbiota, and acidic pH (which does not affect pylori). However, when we experience stress, follow a poor diet, or have difficulty with digestion, we weaken these defenses, making it easier for pylori to take over. This concept applies similarly to other parts of our body such as the intestines, mouth, and vagina. If we develop unhealthy habits, our microbiota suffers and becomes less effective in protecting us as it normally would.
How is my gut health?
I’m leaving you some check-in points so you can evaluate the state of your microbiota (this list is not a medical-level diagnostic, it’s just informative):
- Sadness or bleakness
- Nervousness
- Poor sleep, quality and quantity-wise
- Circadian cycle (in relation to our cortisol levels)
- Focus and memory capacity
- Bowel movements
- Cravings (Is our gut microbiota controlling us?)
The best way to connect symptoms with causes is to keep a journal. Note down what you feel and what have you done that could be the cause. That way you connect that when you drink milk, you need a toilet fast. Don’t go crazy and start recording all your symptoms and leave it in a week. It’s better to do less and be consistent.

How can I improve my gut health?
Gut health depends on a lot of factors, lots of them are habits we can change for our well being. The major factors are: diet, hydration, exercise, stress levels, sleep habits, antibiotic intake, cleanliness, alcohol consumption, and smoking, all impact on the gut. You can find more about them here.
Rome wasn’t built in a day
Be patient. Gut health takes time, you have to discover what works and what doesn’t. When you discover what’s good and implement it, you won’t feel a new person the next day.

Progress isn’t linear
Progress in health habits and results, as in most things, is not linear. You can have downs and ups. It doesn’t matter as long as the overall way it’s up towards your goals.

References
- T. D. Swartz, F. A. Duca, T. de Wouters, Y. Sakar y M. Covasa, «Up-Regulation of Intestinal Type 1 Taste Receptor 3 and Sodium Glucose Luminal Transporter-1 Expression and Increased Sucrose Intake in Mice Lacking Gut Microbiota», British Journal of Nutrition, 107, n.º 5, marzo de 2012, pp. 621-630, doi:10.1017/S0007114511003412.
- Cryan, John F., et al. La revolución psicobiótica: La nueva ciencia de la conexión entre el intestino y el cerebro. España, RBA Libros, 2020.

Leave a comment